Forms
Appeals & Grievances
Online Fillable Form
We make using your dental benefits easy. Browse our library of member forms and documents to find important resources you may need to manage your Delta Dental of Arizona plan. Additional forms may be available in the member portal. If you still can't find what you're looking for, please feel free to contact us.
Forms
Online Fillable Form
Online Fillable Form
Downloadable Form
Downloadable Form
Downloadable Form
Downloadable Form
Additional Resources & Documents
Informational Flyer
Informational Document
Informational Document (updated monthly)
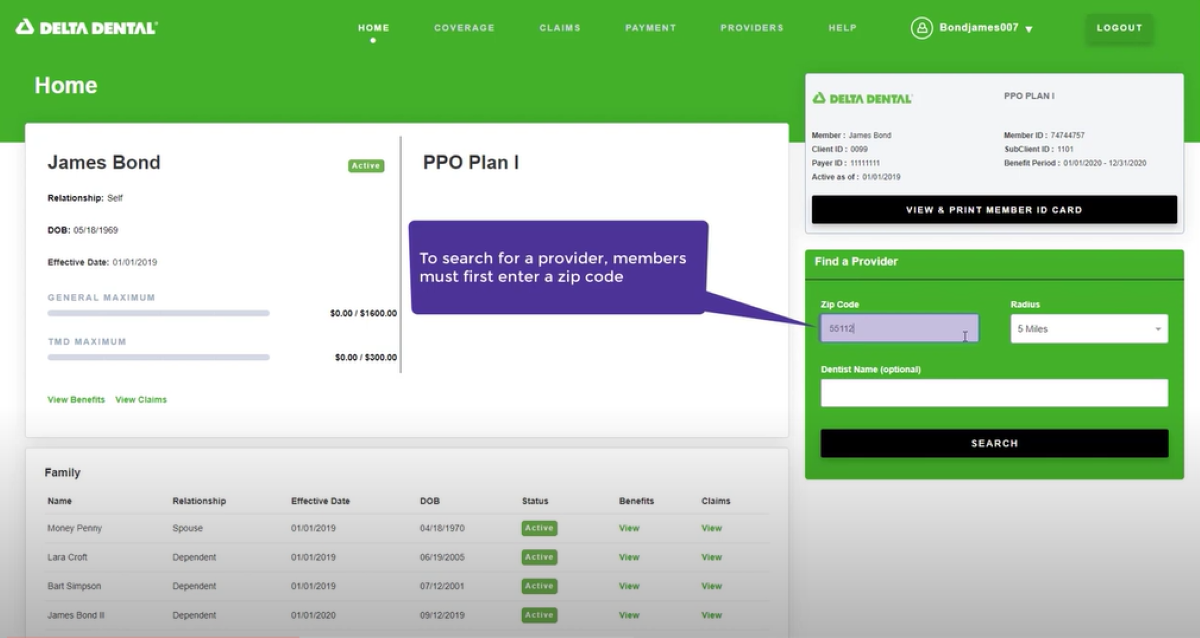
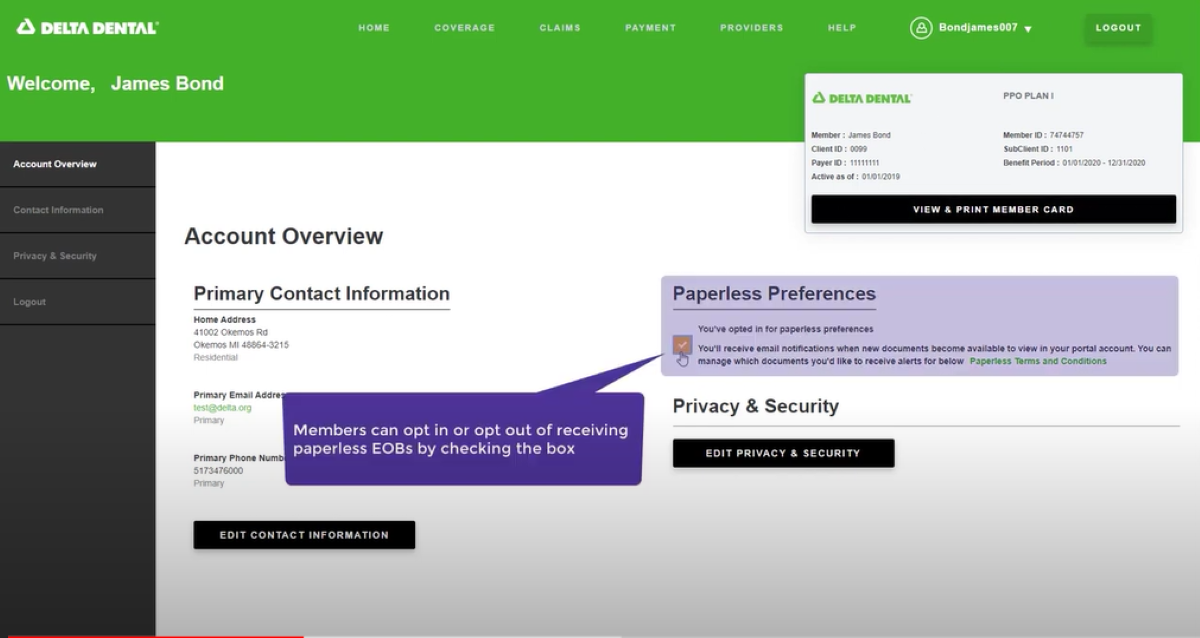
Member Portal Demo Videos
Note: The following videos do not contain sound.
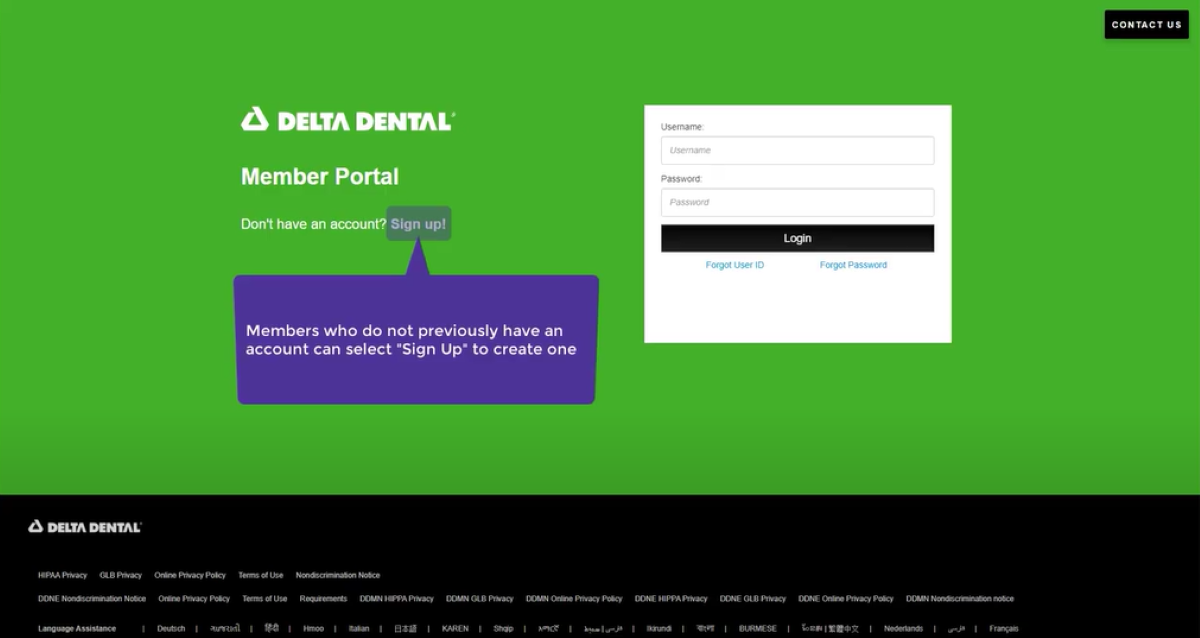
Creating a Member Portal Account
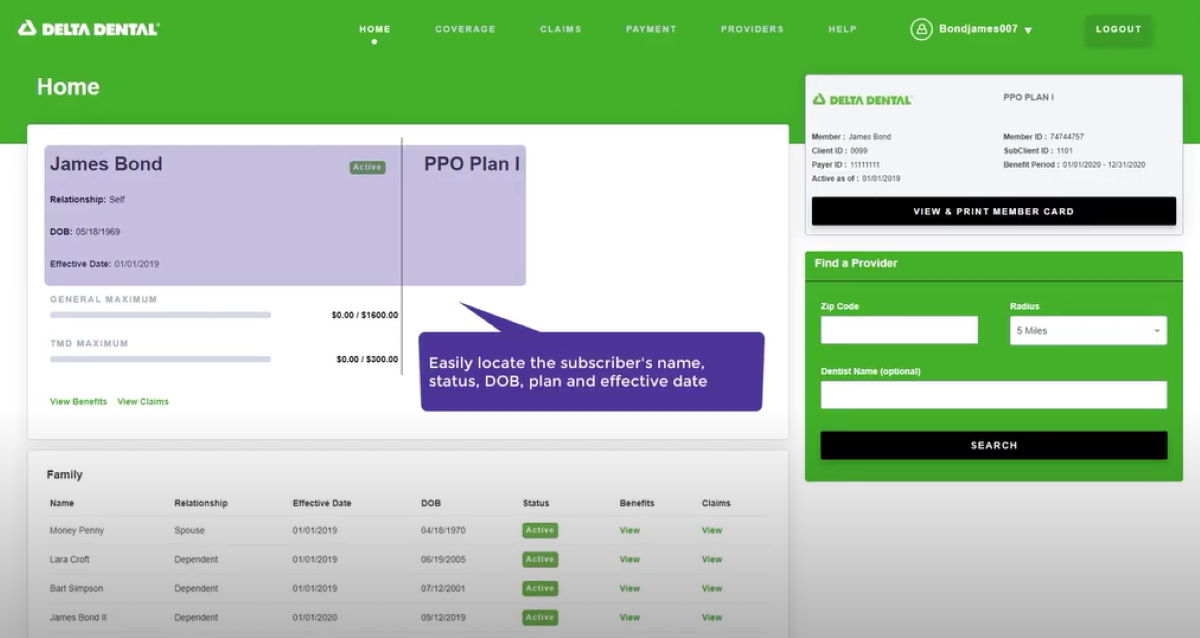
View Benefits & Eligibility
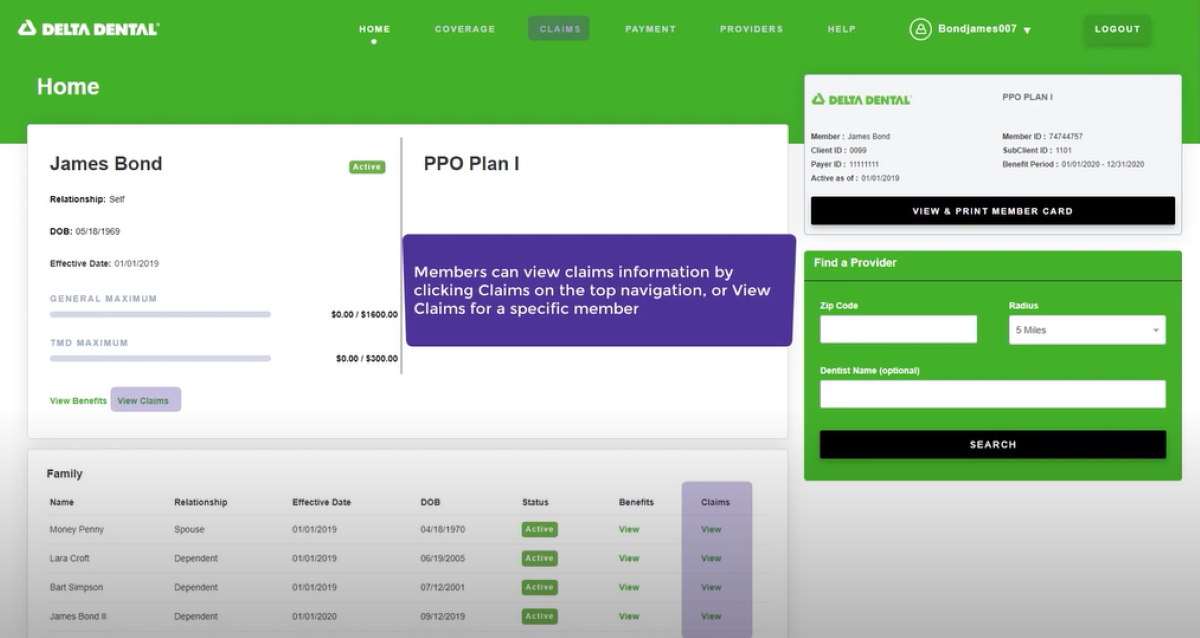
View Claims
View/Print ID Cards
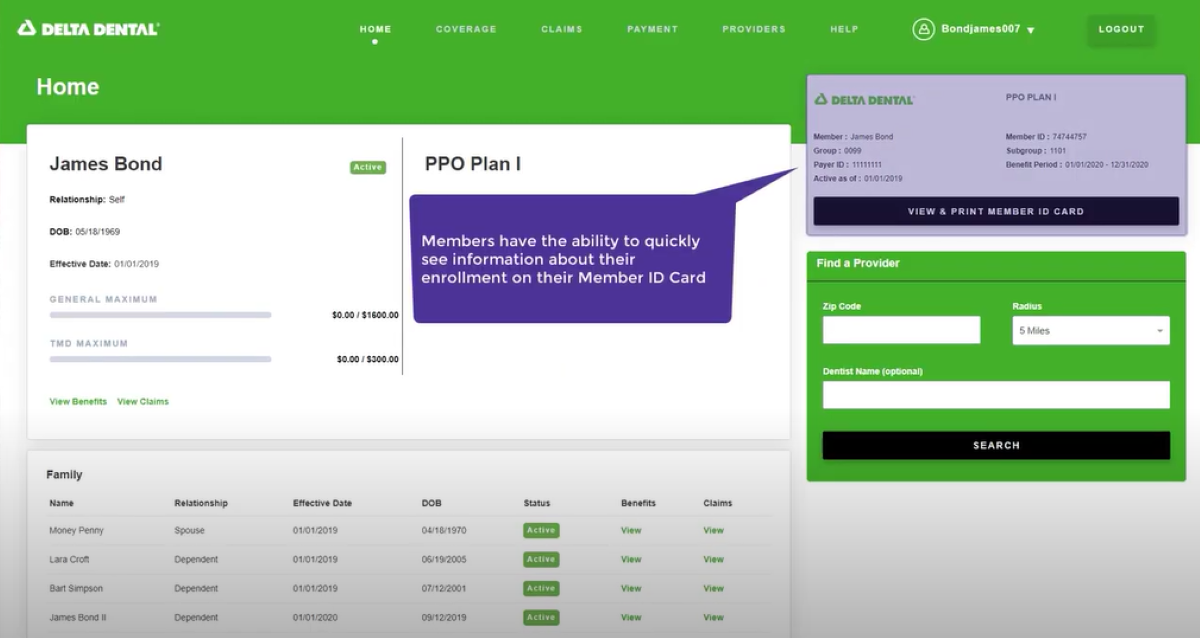
Finding a Network Dentist
Update Account Information
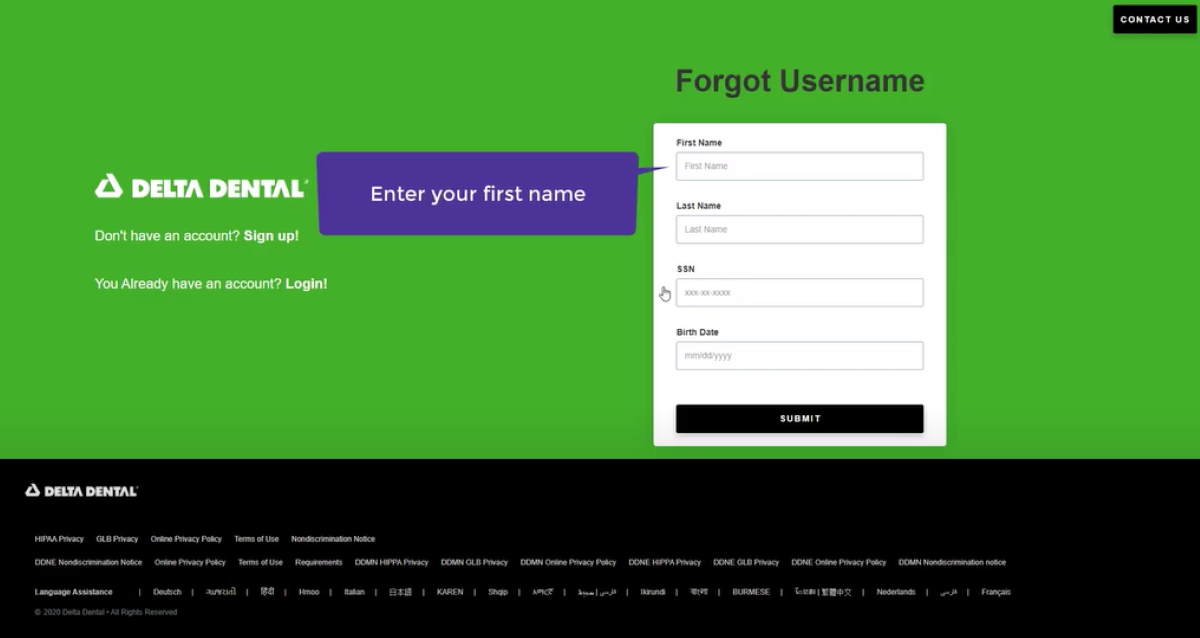
Forgot Username/Password